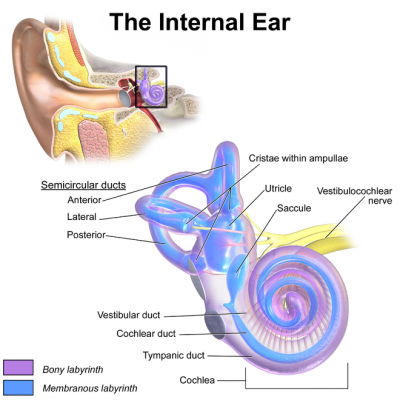
Vertigo in a patient can present due to a number of different causes. The vestibular system includes the parts of the inner ear and brain. These areas process the sensory information involved with controlling balance and eye movements. If disease or injury damages these processing areas, vestibular disorders can result. Vestibular disorders can also result from or be worsened by genetic or environmental conditions, or occur for unknown reasons.
Here at PMPP we treat mainly BPPV-related vertigo. These blogs provide a thorough description of what this involves:
- https://portmelbournephysio.com.au/vertigo-a-case-study/
- https://portmelbournephysio.com.au/vertigo-bppv/
Potential other causes of vertigo and how they can present:
These conditions are managed by medical professionals such as General Practitioners, Neurologists, Ear Nose and Throat specialists, Psychologists, Physiotherapists and more.
1. Peripheral/otological conditions. These are within the inner ear organ or peripheral nerve that innervate that organ.
Vestibular neuritis (hearing preserved) and Labrynthitis (hearing loss):
These are disorders resulting from infection (usually viral infection rather than bacterial). This inflames part of the inner ear organ or nerves connecting the inner ear to the brain.
These commonly have very acute symptoms followed by a resolution of symptoms or chronic symptoms due to damage caused by the inflammation. In the acute phase, symptoms are spontaneous & aggravated by head movements. Symptoms will improve over days and after a few weeks, symptoms will only be present with fast head movements. In the sub-acute to chronic phase symptoms may continue in dark or visually-busy environments.
Characteristics include acute vertigo, disequilibrium (impaired balance or gait, wobbly, sense of unsteadiness), nausea and vomiting, blurred vision, oscillopsia (still objects seeming to jump/jiggle or vibrate), and in the case of labyrinthitis hearing loss and tinnitus (ringing in the ears).
Meniere’s Disease:
Meniere’s Disease a longstanding inner ear disorder. It results from abnormal amounts of fluid called endolymph collecting in the inner ear. The fluid causes increased pressure within the inner ear. The exact cause is unknown and some medication can help. Is characterised by 20 minutes to multiple hours (but <24hrs) of aural fullness (pressure in the ears), fluctuating hearing loss, tinnitus and vertigo (may be spontaneous). There not not usually any symptoms between episodes. Is progressive with progressive hearing loss and motion sensitivity. Meniere’s Disease may progress to both ears.
Acoustic neuroma / schwannoma:
This is a benign tumour that develops from the balance and hearing nerves supplying the inner ear. As it grows, it compresses these nerves usually causing one sided hearing loss, tinnitus (ringing in the ear) and dizziness and loss of balance.
Ototoxicity (oto = ear, toxicity = poisoning):
Is inner ear-related nerve damage that results from exposure to drugs or chemicals that damage this area. Balance and hearing is often impaired and this condition can be temporary or permanent.
BPPV (Benign paroxysmal positional vertigo):
BPPV is characterised by a sudden dizziness that is described by a hallucination of movement (commonly rotatory) that lasts for seconds. This is brought on by head positioning and symptoms are faster resolved by focusing on an object. Severe nausea and vomiting are common and balance is often affected.

2. Neurological/central conditions (within the brain/spinal cord):
Vestibular migraine “dizziness & migraine”:
A migraine is characterised by the following:
- Severe, one-sided, progressive, throbbing or pounding headache.
- Photophobia (sensitivity to light).
- Phonophobia (sensitivity to sound).
- Nausea & vomiting.
- Anxiety.
Prior to, during or after this migraine episode, vestibular (vertigo or balance) symptoms can occur including spontaneous or positional vertigo. Triggers for migraines can include, but are not limited to your environment such as food, drink, hormonal, sleep, stress and weather.
Vertebrobasilar insufficiency (VBI):
VBI occurs when the vertebral and basilar arteries’ blood flow that supply the hindbrain are restricted. This is a common cause of vertigo in the eldery but can occur earlier in life due to vertebral artery dissection (tear). VBI can be related to movement and positions of the neck. On positioning people can display the “5 D’s” or “3N’s”. These include:
- Dizziness.
- Spontaneous nystagmus (uncontrolled and repetitive eye movements, not provoked by movement). This does not setting within a few seconds.
- Feeling faint/unwell.
- Diplopia (double vision & visual field loss).
- Difficulty with speech or finding words.
- Difficulty swallowing or unexplained hoarse voice.
- Sudden collapse without loss of consciousness.
- Nausea & vomiting.
- Numbness or altered sensations around the mouth or nose.
Multiple sclerosis (MS):
Dizziness can be a common symptom for people with MS. It is often described it as a feeling of off balance or lightheadedness rather than ‘the room is spinning’ i.e. vertigo. These symptoms are due to lesions that help with the balance system.
Traumatic brain injury (TBI) due to concussion:
TBI can result in abnormal vestibular function leading to symptoms of dizziness, nausea and brian fog.
3. Other (non-vestibular):
Anxiety:
Anxiety can be characterised by shortness of breath, palpitations, sweating and dizziness.
Cervicogenic dizziness (dizziness originating from the neck):
This is thought to be uncommon and is difficult to diagnose. Many people experience neck pain and dizziness but it can be difficult to tell if they are related or just coincidental. Diagnosis can occur once other causes have been ruled out. As neck pain improves, dizziness often improves. Symptoms often last minutes to hours.
Medication side effects.
Postural hypotension:
Postural hypotension is a form of low blood pressure characterised by lightheadedness/feeling faint when changing positions. change of positions. This may be when moving from lying to sitting or sitting to standing.
References:
- APA Clinical guide to safe manual therapy practice of the cervical spine (part 1) (Thomas L., et al).
- https://www.nationalmssociety.org/Symptoms-Diagnosis/MS-Symptoms/Dizziness-and-Vertigo
- https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/
If you are unsure as to whether Physiotherapy may be able to help your dizziness, contact reception to enquire: https://portmelbournephysio.com.au/contact-us/
~ Lucy Bowden
Physiotherapist

