What is pelvic girdle pain and how common is it?
Pelvic girdle pain (PGP), also commonly referred to as Pelvic instability, can be described as a collection of signs and symptoms of discomfort and pain in the pelvis and lower back region. Pain can either be felt at the back of the pelvis, on one or both sides, and/or pain over the pubic symphysis.
Pain may also be referred into the buttock, groin, inner thigh and perineum. Symptoms vary from mild discomfort to severe pain that can hinder mobility. As many as 50% of women experience PGP during pregnancy. 90% of women recover from PGP within 12 months of having their baby. However, up to 10% of women can continue to have significant PGP and disability 2 years post-birth.
What causes PGP during pregnancy?
The development of PGP during pregnancy is multifactorial. This can be related to the following factors:
- Hormonal.
- Biomechanical.
- Traumatic.
- Genetic.
- Metabolic.
- Degenerative.
During pregnancy there are many physical changes that occur to the way your body works:
- Your tummy growing, stretching your abdominal and stomach muscles.
- The increasing pressure on your pelvis, and pelvic floor, due to the increasing growth of your uterus and baby.
- Changes in your centre of gravity and posture, as your tummy grows. This leads to increased stress/strain on your lower back and pelvis.
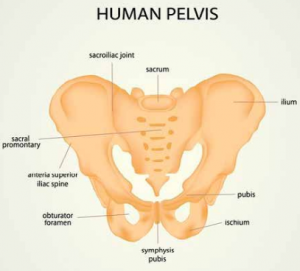
Image credit: https://www.fitwise.com.au/pelvic-girdle-pain-during-pregnancy/
Other reported risk factors include the following:
- Previous pelvic or lower back pain and/or history of trauma to the pelvis and lower back.
- Increased number of previous pregnancies.
- Physically demanding work.
- High bodymass index (BMI).
- Emotional distress.
- Smoking.
Pain might be associated with:
- Getting in and our of bed or car.
- Rolling in bed or lying flat on your back.
- Standing on one leg, e.g. getting dressed or getting into the car.
- Driving a manual car.
- Prolonged sitting or standing, or moving from sitting to standing.
- Walking, going up down stairs, lunging or squatting.
- Bending and lifting heavy objects/other children.
- Housework.
- High impact activities, such as running and jumping.
Managing your pelvic girdle pain:
Tips to avoid increasing your pelvic girdle pain include:
- Reducing non-essential weight-bearing activities such as climbing stairs, standing/walking for long periods of time. This may mean modifying exercise. Take smaller steps and walk shorter distances if you are able to, without increasing your pain. Also try to avoid walking on uneven or soft surfaces.
- Prioritise horizontal rest.
- Avoid activities which involve standing on one leg, e.g. sit down to get dressed.
- Keep your knees together when rolling in bed/getting out of bed or the car.
- Break up larger tasks into smaller activities.
- Avoid repetitive and heavy bending tasks.
Remaining active during pregnancy is key to managing your overall health and pelvic girdle pain during pregnancy. Some examples of safe exercise include swimming, cycling, Clinical Exercise/Pilates classes, gym/strength training and Yoga.
Treatment options for PGP:
Physiotherapy treatment can be effective in reducing the symptoms of PGP. The following options have been found to improve functional outcomes and reduce pelvic girdle pain during pregnancy:
- Manual therapy.
- Provision of pelvic support garments.
- Advice regarding correct and safe exercise.
While symptoms can be similar from person to person, the underlying cause can vary and thus treatment must be tailored to the individual.
PGP treatment often will include:
- Education about appropriate postural changes/positions to relieve pain. It may also include other pain management strategies such as ice/heat, stretching and use of spikey ball.
- A specific exercise program to strengthen postural, core and pelvic floor muscles.
- Hands-on treatment to relieve stiff, painful joints and muscles.
- Advice on external support garments such as Tubigrip and other pregnancy pelvic support garments (SRC/Lenny Rose maternity shorts/leggings) or a Sacroiliac/Pelvic belt.
- Our Clinical Exercise classes may be recommended to you to address any underlying muscle weakness or asymmetry. These classes are very popular amongst our PMPP pregnancy community! Learn more here: https://portmelbournephysio.com.au/pregnancy-postnatal/
- Traditional Chinese Medicine Acupuncture has also been shown to be effective in managing the symptoms of PGP.
If you are experiencing signs and symptoms of PGP during your pregnancy, please do not hesitate to book an appointment with one of our experience Physiotherapists at PMPP. They will help tailor and guide your management throughout your pregnancy journey.
~ Diana Emmerson
Physiotherapist
Search the Lenny Rose Active range here and use code PORTMELBOURNEPHYSIO to get 15% off: https://lennyroseactive.com.au
We stock a range of SRC antenatal and postnatal products in the clinic.
We advise consulting with one of our Physiotherapists prior to purchasing garments to ensure the best fit and most suitable product.
You may find these other related PMPP blogs interesting:


