Drawing on personal experience:
When considering becoming qualified in Pelvic Health Physiotherapy, I reached out to my good friend and sounding board, Rosie. “Ali, I have an exercise for you”. She told me. “Write down every single thing that you have experienced firsthand, that you are likely to see in a patient presenting for a Pelvic Health consultation”.
Before I knew it, I had written down, in no particular order, everything I have been through pertinent to this area of Physiotherapy:
- Mastitis (not directly Pelvic Health but often coexists).
- Urogynaecology consultations with urodynamic testing and pelvic ultrasounds.
- Fertility treatment.
- Vaginal birth with an epidural, forceps and episiotomy.
- Elective caesarean section delivery.
- Vulvar varicosities.
- Anterior and posterior vaginal prolapses.
- Use of estrogen cream.
- Pelvic floor trigger point release.
- Haemorrhoids.
- Stress urinary incontinence and the use of incontinence products.
- Postnatal depression.
- Pessary use (four different types).
- Pelvic pain.
- Constipation management.
- Filling out a bladder diary.
- Pelvic floor muscle uptraining.
- Pelvic floor down training.
- SIJ dysfunction and use of an SIJ belt.

Written down like this, it made perfect sense to me why I was so drawn to this area of my profession. I live and breathe pelvic floor dysfunction on a personal basis every day and have done so for four years.
Stress urinary incontinence: the diagnosis that has changed my life.
Of all the above mentioned issues/procedures/
What are the causes of SUI?
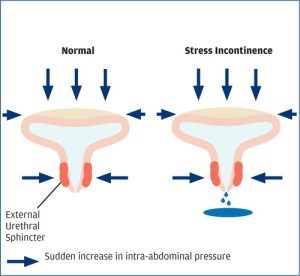
SUI arises when the pressure above the urethra (the tube that allows urine to pass outside the body) is greater than the pressure below. Intra-abdominal pressure (IAP) is generated with coughing, sneezing, laughing, vomiting, heavy lifting or impact exercise i.e. running, jumping or skipping. This needs to be mitigated with good closing pressure at the level of the urethra.
Two causes of this insufficient pressure are:
- Urethral hypermobility (excessive movement of the urethra which allows urine to leak through).
- Intsrincic urethral sphincter deficiency: the sphincter (a muscular structure that keeps urine in the urethra) is not able to generate enough resistance/pressure to keep urine from leaking out.
For some women, this can be merely an annoyance. For others, it can be literally crippling. I have always identified as a runner. It is something I have done since my teenage years for my physical fitness and mental wellbeing. Despite trying swimming, cycling and other forms of cardio exercise, the endorphins and clarity of thinking are, for me, unique to this sport.
It felt like my body had failed me:
Following Claudia’s delivery in 2020, I developed SUI with running. In 2017 I ran a full marathon without a toilet stop. 42km without single drop of leakage. To have this happen to me felt like a real blow. With extensive Physiotherapy input, I had a mild improvement in symptoms but when I fell pregnant with Georgina in 2021, this fell by the wayside. I have been incontinent with running ever since. This is regardless of what I drink prior, the time of day or how far I run.
Let’s look at the research:
Following the Women’s Health Training Associates 2023 research update, “1/3 to 1/2 of all women can completely stop their urinary incontinence after completing a three month intensive pelvic floor muscle training program and 75-80% experience some, if not major improvement’.
Historically, surgery has been the only option for SUI. Aside from the usual surgical risks, it is not a given that the SUI will be completely corrected. It makes me so excited to see this research. To know that, as Pelvic Health Physiotherapists, we can enable a woman to regain freedom from this debilitating condition.

A shameful secret for many but I am doing my best to change that:
Many women suffer in silence with SUI. It is incredibly embarrassing to lose continence with things like laughing, coughing or exercising. I have been inspired by other movers and shakers in this space. Women who feel comfortable sharing their story and spreading a message of hope. No longer do we have to put up with SUI as ‘just part and parcel’ of being a woman. It starts, like all things that require vulnerability, with a conversation. I understand the indignity that comes with this condition all too well and am determined to lessen the shame and stigma attached.
After exhausting all conservative measures . . .
Unfortunately, I am one of the 20-25% who has exhausted all conservative options and will require surgery later this year. The plus side? I will be able to add another item to my ‘firsthand experience’ list. Ever the optimist. I will also be having prolapse surgery at the same time – a separate procedure but one that often coexists with SUI.
If you or someone you care about is struggling with SUI, please reach out. Alex, Emily, Julia (currently on maternity leave) and I have a myriad of tools that can, and almost always do, help.
Yours in health,
Ali
Other PMPP blogs that you may find interesting:
- https://portmelbournephysio.com.au/exercising-during-pregnancy/
- https://portmelbournephysio.com.au/pelvic-girdle-pain-in-pregnancy/
- https://portmelbournephysio.com.au/mental-health-and-pelvic-floor-dysfunction/
- https://portmelbournephysio.com.au/the-overactive-pelvic-floor/
- https://portmelbournephysio.com.au/pelvic-pain-awareness-month/
Continence Foundation of Australia: https://www.continence.org.au


