What is plantar fascia?
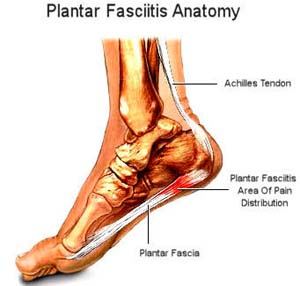
Plantar fascia is a band of collagenous connective tissue found in the foot. It is attached to the bone located at the heel of the foot (the calcaneous) and inserts into the base of the big toe (the first metatarsal).
The plantar fascia forms the medial longitudinal arch of the foot. It has an important role in providing support and shock absorption. Additionally, it assists the foot during walking, particularly towards the end stage of stepping. It ensures the foot is stable and helps to offload tension and stress from the ligaments and other structures of the foot.
What is Plantar Fasciitis?
Plantar fasciitis is an inflammatory, overuse injury of the plantar fascia caused by disarray of the collagen fibres. Symptoms of plantar fasciitis include;
- Gradual onset of heel pain (particularly the medial/inside of the heel)
- The pain is worse in the morning and gets better during the day. However it flares up again at night time.
- Decreased flexibility and strength of calf, hamstring and gluteal muscles.
What are the risk factors of Plantar Fasciitis?
- When the arches of the foot are too high, the foot is in too much supination and this causes increased strain on the plantar fascia.
- Conversely, when the arches of the foot are too low, the foot is over-pronated and this also causes excessive strain on the plantar fascia.
- Wearing non-supportive or inappropriate footwear can alter the biomechanics of the lower limbs and place many structures at risk of injury, including the plantar fascia.
- If you have an increased body mass index (BMI) this can increase the stress and strain on many structures of the body and particularly the plantar fascia due to increased forces going through the foot.
- A reduced ankle dorsiflexion (bending the ankle upwards) range of motion can increase the risk of plantar fasciitis. If the ankle is not able to move freely throughout it’s normal range of motion, neighbouring structures, for example the plantar fascia, will try to compensate and therefore can become tight and inflamed.
- Tight and weak calf, hamstring and gluteal muscles can also alter the biomechanics of the lower limbs and place the plantar fascia at risk of becoming inflamed.
- Evidence suggests that if you are weight bearing, for example standing and walking a lot during the day, then you are also at an increased risk of plantar fasciitis.
How is Plantar Fasciitis diagnosed?
The most effective imaging to diagnose plantar fasciitis is ultrasound. It is a non-invasive and relatively quick investigation. If you think you might be experiencing the above symptoms, please discuss this with your physiotherapist and they can give you further information in order to organise an ultrasound if required.
What are the best treatments available for Plantar Fasciitis?
Your physiotherapist will guide you through the treatment process which will involve some of the below techniques;
- Initially you will be asked to avoid anything that aggravates the pain
- Ice to assist with the inflammation
- Exercises to improve the flexibility of your calf muscles & stretch the plantar fascia
- Massaging the plantar fascia and you can practise this at home by rolling the soles of your foot and heel over a small ball (e.g. golf ball) or a frozen water bottle.
- Massage of other tight lower limb muscles.
- Taking non-steroidal anti-inflammatory drugs (NSAID) can assist with the inflammatory process. Discuss this with your physiotherapist or general practitioner.
- Taping the foot to offload the plantar fascia and assist with your pain management.
- You may require orthotics and a review of your footwear to assist with the arches in your foot and to normalise your biomechanics.
- Placing silicone gel heel pads in your shoes may help with your pain management.
- Completing strengthening exercises for your hip, knee and ankle muscles will ensure effective use of the muscles and decrease the stress on the plantar fascia.
- Education will be provided, as required, regarding ways to decrease your BMI and a referral to a nutritionist may be provided.
- Clinical Pilates will assist with improving your flexibility and the strength of your lower limbs whilst simultaneously improving your core stability. It will also assist with future flare ups of your plantar fasciitis.
- There is some evidence to support the use of extracorporeal shock wave therapy for short term pain management in clients experiencing chronic plantar fasciitis however it is unclear about the longer term benefits.
- If your pain continues to persist after applying the above treatment techniques, you may be required to wear night splints, have a corticosteroid injection or surgery to release the plantar fascia. Your physiotherapist will discuss these techniques with you if required.
– Julia Esposito
References:
- Brukner & Khan “Clinical Sports Medicine” Fourth Edition. (2012). pg 847-850.
- Riddle, D.L., Pulisic, M., Pidcoe, P., Johnson, R.E. (2003). Risk Factors for Plantar Fasciitis: A Matched Case-Control Study. J Bone Joint Surg Am 85 (5): 872 -877
- Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM. (2014). Heel pain-plantar fasciitis: clinical practice guidelines linked to the International Classification of Functioning, Disability and Health from the Orthopaedic Section of the American Physical Therapy Association. The Journal of Orthopaedic and Sports Physical Therapy 44(11):A1-A33. Practice guideline
- Podolsky R, Kalichman L. (2015). Taping for plantar fasciitis. Journal of Back and Musculoskeletal Rehabilitation 28(1):1-6. Systematic review
- Yin M-C, Ye J, Yao M, Cui X-J, Xia Y, Shen Q-X, Tong Z-Y, Wu X-Q, Ma J-M, Mo W. (2014). Is extracorporeal shock wave therapy clinically efficacy for relief of chronic, recalcitrant plantar fasciitis? A systematic review and meta-analysis of randomized placebo or active-treatment controlled trials. Archives of Physical Medicine and Rehabilitation. 95(8):1585-1593. Systematic review
- Macintosh Lower Limb Clinic. Retrieved 28/08/15 via http://www.macintoshlowerlimbclinic.com.au/conditions-treated/fact-sheets.html